What Are The 4 Stages Of Congestive Heart Failure
Discover the 4 stages of Congestive Heart Failure (CHF) and learn how to recognize symptoms, seek timely treatment, and improve your quality of life.
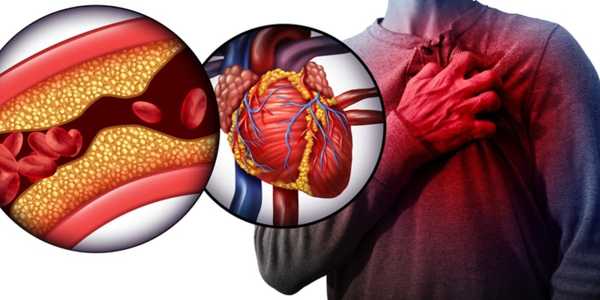
Congestive heart failure (CHF) is a chronic condition wherein the heart struggles to pump blood effectively, leading to various health complications. This progressive disease can greatly diminish an individual's quality of life, making it essential for both patients and healthcare providers to understand its stages fully. Recognizing the different stages of CHF facilitates timely medical intervention and empowers patients to make informed decisions regarding their treatment and lifestyle adjustments.
Understanding Congestive Heart Failure

Congestive heart failure (CHF) is a complex, chronic syndrome characterized by the heart's inability to pump blood efficiently. This inefficiency leads to reduced blood flow to vital organs and fluid accumulation in various body tissues, resulting in shortness of breath, fatigue, and swelling in the legs and abdomen. The dysfunction is primarily attributed to a weakened heart muscle that struggles to maintain sufficient cardiac output necessary for the body's metabolic requirements.
Multiple causes and risk factors contribute to the onset of CHF. High blood pressure (hypertension) is a significant contributor, adding stress to the heart as it must work harder against elevated vascular resistance. Additionally, diabetes can damage both heart tissue and blood vessels, further complicating cardiovascular health. Lifestyle choices such as poor diet, lack of physical activity, smoking, and excessive alcohol consumption elevate the risk of CHF. Understanding these risk factors is vital, as they underscore the necessity for preventive measures and effective management strategies in combating the disease.
The Four Stages of Congestive Heart Failure
Congestive heart failure (CHF) has four distinct stages, each representing a different level of heart function and symptomatology. Recognizing these stages allows patients and caregivers to manage the condition more effectively. Below, we discuss the characteristics and implications of each stage.
Stage A: At Risk but Not Developing Symptoms
In Stage A of CHF, individuals are identified as at risk for developing heart failure due to prevalent risk factors like hypertension, diabetes, and a familial history of heart disease. Although there are no observable symptoms or functional limitations at this stage, it is a crucial indication for intervention. The heart remains structurally healthy; however, risk factors may predispose individuals to future heart failure. At this juncture, the focus should be on lifestyle modifications to mitigate risks, including maintaining a healthy weight, managing blood pressure, and committing to regular physical activity. These proactive measures are crucial to prevent progression to severe stages of heart failure.
Stage B: Asymptomatic Heart Failure
Stage B involves individuals with structural heart disease, which can be identified through diagnostic imaging techniques despite the absence of symptoms and functional restrictions. Patients may show abnormalities such as left ventricular hypertrophy or a history of myocardial infarction. Regular life can continue without overt signs of heart failure, making this stage particularly deceptive. Diagnostic imaging like echocardiograms and stress tests become essential in recognizing Stage B, often allowing detection even before symptoms appear. Treatment in this phase typically includes medications like ACE inhibitors or beta-blockers to manage existing risk factors and minimize the likelihood of progression to symptomatic heart failure. Consistent monitoring by healthcare professionals is vital to sustaining heart function effectively.
Stage C: Symptoms and Structural Heart Disease
At Stage C, patients begin to experience more pronounced symptoms associated with CHF. Common complaints include shortness of breath, tiredness during physical activities, and swelling in the legs, ankles, or abdomen due to fluid retention. These symptoms can profoundly impact daily life, making routine tasks increasingly difficult and preventing individuals from participating in social activities. The psychological effects of living with CHF can lead to anxiety and depression, further complicating the overall quality of life. Simple activities like going up stairs or walking short distances often become challenging. Management of Stage C involves implementing lifestyle changes, prescribing diuretics to alleviate fluid retention, and utilizing heart failure-specific medications tailored to the patient's requirements. Close monitoring and potential treatment adjustments are essential to effectively manage symptoms and prevent hospitalizations.
Stage D: Advanced Heart Failure
In Stage D, CHF reaches its most critical form, characterized by extreme limitations in physical activity and persistent symptoms that may intensify even during rest. Patients might endure serious fatigue, continual dyspnea, and significant edema, severely affecting their quality of life. At this point, conversations surrounding end-of-life care and palliative treatment options become increasingly relevant. Management strategies might involve advanced therapies such as mechanical circulatory support or even heart transplantation, depending on individual circumstances. Additionally, comprehensive palliative care becomes critical, focusing on comfort and dignity for the patient. Educational resources and support systems are integral to navigating the complexities of advanced heart failure compassionately and effectively.
By familiarizing oneself with these stages of CHF, individuals can better recognize symptoms and pursue timely interventions, thus improving their management of this chronic condition.
Importance of Regular Monitoring in CHF
Regular monitoring is vital in managing congestive heart failure (CHF), allowing healthcare providers to detect changes in symptoms and heart function as the disease progresses. Key diagnostic tests include blood analysis to monitor biomarkers like B-type natriuretic peptide (BNP) levels and imaging studies such as echocardiograms that examine heart structure and performance. These evaluations are essential for assessing treatment effectiveness and adjusting medications to ensure optimal health outcomes. Furthermore, routine physical assessments that track vital signs and overall health contribute to a comprehensive grasp of a patient's condition. By utilizing these diagnostic tools, healthcare teams can identify deteriorating heart failure early, preventing complications and enhancing overall quality of life. Regular check-ups empower patients through awareness of their health status, ultimately guiding them towards informed choices in managing CHF effectively.